We catch up with Healthy Eating DR founder, Dr  Harriet Holme, who explains why the bacteria in breastmilk are so vital for the health of our small humans.
Harriet Holme, who explains why the bacteria in breastmilk are so vital for the health of our small humans.
As a mother of two children, I know from personal experience that breastfeeding can be tough and demanding but also very rewarding. As a former paediatrician, I’m a strong advocate for mothers to be supported without judgement however they chose to feed their baby. Equally, I do think it is vitally important for mothers to have unbiased, science backed information so that they can make an informed choice about feeding. There are a number of key reasons how breast milk is different to formula milk, and I’ll talk through why this is important. Even more astonishingly, there is even a difference between the microbiota in pumped breast milk and the bacteria in breast milk from direct transfer from the breast. Find out if mix feeding matters. Learn about the differences between mix feeding, breastfeeding, and how formula milk change the infant microbiota.
What is the microbiota?
While some bacteria are harmful, many are key to our health. The microbiota is the term used to cover the trillions of bugs, mostly made up of bacteria, that live on our skin and in our gut. The microbiome is the genetic content of these microorganisms.
Why is the microbiota important?
We know that these single cell organisms play a huge role in many aspects of our health as adults, ranging from reduced risk of type 2 diabetes, obesity, immune function and even response to chemotherapy1.
How is the infant microbiota formed?
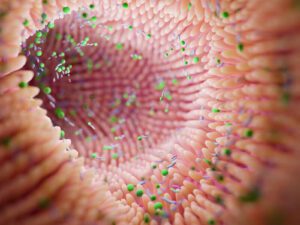 When breastfeeding, the mother and baby although individuals, have an interactive relationship, that is called a dyad; this is highlighted by how the friendly microorganisms in breastmilk (milk microbiota) are formed. A healthy gut microbiome was first thought to be established by exposure through vaginal delivery and secondly through transfer of bacteria through breastmilk1,2 but there is now evidence that this is simplified, with many additional factors playing a role2.
When breastfeeding, the mother and baby although individuals, have an interactive relationship, that is called a dyad; this is highlighted by how the friendly microorganisms in breastmilk (milk microbiota) are formed. A healthy gut microbiome was first thought to be established by exposure through vaginal delivery and secondly through transfer of bacteria through breastmilk1,2 but there is now evidence that this is simplified, with many additional factors playing a role2.
Live microorganisms are already found in breastmilk, even before a mother has breastfed her baby for the first time, providing evidence of maternal origin (called entero-mammary pathway)2. The microorganisms in the baby’s mouth are similar to the mother’s breastmilk. New evidence suggests that in addition to maternal transfer, there is also communication via the baby’s saliva back into the breast, which also has a role in determining the infant microbiota 2
Mode of delivery, older siblings, maternal and infant antibiotic exposure, complementary feeding with formula milk, and even mode of feeding (pumped breastmilk versus directly at the breast) are all thought to play a part in determining the baby’s gut microbiota2. Some of these factors may only act in the short term, for example there is some evidence to suggest that mode of delivery has no persistent effect at 8 months3. While others may have a more long term effect on the infant microbiota, for example, stool microbiota profiles of children at 1 year were significantly different in those that were still breastfed, compared to those that weren’t4. This was independent of previous antibiotic exposure or mode of delivery4. More research is still needed to determine why the microbiota is different with pumped breastmilk compared with direct transfer, to answer whether it is the act of pumping or lack of contact with the baby’s mouth2.
Ultimately whether breastmilk provides the microorganisms to colonise the baby’s gut, or provides nutrients and prebiotics to foster a specific environment for selective growth of certain microorganisms, or a mixture of both, has yet to be fully established2. However, maturation and maintenance of the lining of the infant gut depends on bacterial colonisation5 and with evidence to support a long term health impact2,6,7.
Why is breastmilk different?
Breastmilk contains a number of different components that make it different to formula milk, that are hard to replicate. In addition to the microorganisms, other components of breastmilk such as immune cells, fatty acids, antibodies, and human milk oligosaccharides (HMOs), also have a role in shaping the diversity of organisms in the infant microbiota 2.
Human milk oligosaccharides
Human milk oligosaccharides (HMOs) are short chain carbohydrates, which are present in breastmilk that are essentially undigested by the baby, but are an important nutrient source for specific types of bacteria in the gut, called prebiotics8. One of the bacteria commonly seen the gut of healthy babies is Bifidobacterium longus infantis that metabolise HMOs into acetate and lactate9. These compounds are acidic, and change the pH of the infant stool, which are associated with lower levels of potentially harmful bacteria and those that harm the lining of the gut9. The formation of other bacteria that are potentially harmful, maybe prevented by HMOs, thereby shaping the formation of the microbiome, improving the barrier function of the lining of the gut, and playing a role in immune function8.
are essentially undigested by the baby, but are an important nutrient source for specific types of bacteria in the gut, called prebiotics8. One of the bacteria commonly seen the gut of healthy babies is Bifidobacterium longus infantis that metabolise HMOs into acetate and lactate9. These compounds are acidic, and change the pH of the infant stool, which are associated with lower levels of potentially harmful bacteria and those that harm the lining of the gut9. The formation of other bacteria that are potentially harmful, maybe prevented by HMOs, thereby shaping the formation of the microbiome, improving the barrier function of the lining of the gut, and playing a role in immune function8.
Lactoferrin
Lactoferrin, found in breastmilk, binds iron for transfer and aids it’s absorption through the infant gut lining8. This has a duel role, firstly helping the baby to absorb and use this iron as an important nutrient, and also leading to a reduction of the quantity of iron in the gut, which prevents harmful bacterial growth8.
Antibodies in Breastmilk
 Antibodies are used to tag microbes like viruses and bacteria, for destruction by other immune cells. Levels of certain antibodies (IgA, IgG and IgM), have been found to be higher in the guts of babies who are breastfed10. When babies are born, they are initially unable to produce the antibodies they need.
Antibodies are used to tag microbes like viruses and bacteria, for destruction by other immune cells. Levels of certain antibodies (IgA, IgG and IgM), have been found to be higher in the guts of babies who are breastfed10. When babies are born, they are initially unable to produce the antibodies they need.
Breastmilk functions to supply these antibodies for the first few weeks until the baby is able to produce enough themselves10. Supply of antibodies from breastmilk means that babies who are breastfed, have a lower risk of some childhood infections8.
Low levels of antibodies (specifically IgA), as a baby has been associated with increased risk of development of allergies and asthma during childhood11, and development of Crohn’s disease (chronic inflammatory condition of the gut), in children12.
Xanthine oxidase
Interestingly breastmilk contains an enzyme called xanthine oxidase, while neonatal saliva contains the substrates for this enzyme (xanthine and hypoxanthine). When the enzyme mixes with these substrates in the mouth and intestinal tract of the baby, a chemical reaction occurs, releasing hydrogen peroxide. This is antibacterial, and regulates the growth of some bacteria, possibly with a role in creating the different microbiota seen in breastfed babies13.
Does the type of milk matter?
Animal studies in monkeys have found that there are changes in the immune system in exclusively breastfed babies compared to those who are fed formula, and that these changes persist for 3-5 years after birth, long after weaning14.
In humans, gut bacteria have been found to differ between exclusively breastfed and formula fed babies5. Prebiotic like compounds added to formula milk, predict a microbiota distinct to that seen in an exclusively breastfed baby3. While mix fed babies have a microbiota that appears to be on a spectrum between that of breastfed and formula fed babies15.
What about weaning?
Introduction of complementary foods (weaning) changes the microbiota in the baby’s gut. Early weaning starting at 4 months or before, has been associated with a 30% higher risk of being overweight or obese (high Body Mass Index) in childhood, and a less diverse gut microbiota16. A high Body Mass Index (BMI) in childhood is associated with a higher future risk of high cholesterol profile, high blood pressure, diabetes and cardiovascular disease17. However, those children who were breastfed for more than 4 months, did not have a higher BMI at 5 years, regardless of age at weaning16, so breastfeeding appears to be protective.
Are there benefits of breastmilk long term?
The first 1000 days of life is a critical period for development of the immune system4, and up to 70% is associated with the gut18. In the first few months of life, patterns are established for recognising self and non-self (highly important in autoimmune diseases), that have life-long consequences6,7.
associated with the gut18. In the first few months of life, patterns are established for recognising self and non-self (highly important in autoimmune diseases), that have life-long consequences6,7.
There is evidence that the incidence of eczema, and wheezing in the first 2 years of life can be decreased by exclusive breastfeeding for 3 to 4 months19. Additionally, evidence suggests that a longer duration of breastfeeding may protect against asthma after the age of 5 years19. Breastfeeding has not been shown to prevent or delay the onset of specific food allergies19.
Maternal benefits of breastfeeding
For mothers, in addition to the psychological aspect of bonding, breastfeeding decreases the risk of breast cancer and may protect against ovarian cancer and type 2 diabetes20.
Summary
I hope this article has helped to explain about the nutritional differences between breast milk and formula milk with regarding your baby’s microbiota. I’ve explained how breast milk and formula milk are different, and why bacteria in breast milk are so important. The infant microbiota has been shown to have a role in longer term health, but so much more research is needed.
If you are looking for more information about what to eat after a baby and beyond, check out Dr Harriet’s book ‘Postpartum Nutrition: An Expert’s Guide to What to Eat After a Baby‘.
If you are currently breastfeeding, check our Dr Harriet’s FREE meal planner and micronutrient checklist helpful. Dr Harriet created this planner and checklist in an easily accessible format, so that you don’t have to hunt for reliable information to help you eat well during breastfeeding.

